‘Helping Children with ADHD and ASD Sleep was originally published by Mattress Reviews and can be found here‘
Attention deficit/hyperactivity disorder (ADHD) is one of the most common disorders affecting children, with the CDC estimating between 5 to 11 percent of children being affected. While less than 2 percent of children have an autism spectrum disorder (ASD), as many as 50 percent of children with ASD also have ADHD, and children with one or both conditions share many of the same sleep issues.
Below we’ll review the commonalities between these disorders, how to recognize symptoms and receive a diagnosis for your child, and common sleep issues and guidance for helping your child get a better night’s sleep.
How are ADHD and ASD similar, and how are they different?
ADHD and ASD share many similarities, and the conditions are often comorbid with each other. Between 30 to 50 percent of children with ASD also show ADHD symptoms, and two-thirds of children with ADHD display features of ASD. Both disorders are more common in boys than girls, and children with either disorder have difficulty communicating with peers and paying attention, and are prone to impulsivity or restless behaviors. Symptoms of either disorder significantly interfere with a child’s emotional development and performance in school and activities that take place in and outside the home.
However, there are some key differences between ADHD and ASD. When children with ADHD struggle in social environments, it is not from lack of understanding the “rules.” Children with ASD, on the other hand, inherently don’t understand the “rules” and have difficulty recognizing social cues that make the rules apparent. A good example of this distinction is taking turns. A child with ADHD may overstep their bounds or have difficulty waiting for their turn, despite intuitively knowing they should, while a child with ASD does not understand the concept of taking turns altogether.
Both disorders can be diagnosed in early childhood, although ADHD can be more challenging to diagnose since children can similarly act out from being sleep deprived or “just being kids.” Both disorders have varying degrees of severity, which may also impact when the child is diagnosed.
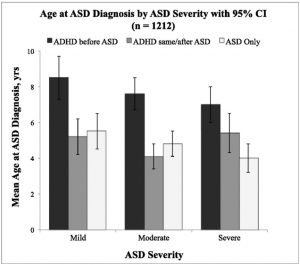
Source: American Academy of Pediatrics
What is ASD?
Previously diagnosed separately under the Diagnostic and Statistical Manual of Mental Disorders (DSM), autism spectrum disorders (ASD) are a group of neurodevelopmental disorders including autism, Asperger’s syndrome, and pervasive developmental disorder not otherwise specified (PDD-NOS). Children with ASD range in intellect from being highly gifted to mentally challenged, but all experience delayed social development and have issues communicating and socializing with others.
For instance, a child with ASD may regularly fail to respond to social invitations or during two-way conversations, have an unresponsive facial expression, avoid eye contact, or display otherwise abnormal social behaviors that make it difficult for them to develop and maintain various social relationships. They may also engage in repetitive behaviors, such as mimicking other’s speech, repeating phrases, constantly lining up objects, or excessive hand-waving.
The Centers for Disease Control and Prevention estimate 2 million Americans have ASD, and it’s nearly 5 times more common in boys than in girls.
Diagnosing children with ASD
Symptoms of ASD show up as early as age 3. The CDC recommends doctors screen children for signs of developmental delays and ASD symptoms during their regular wellness visits at 9 months, 18 months, and 24 or 30 months. Children with other family members of ASD are considered high-risk and may be tested more frequently throughout childhood.
If your pediatrician sees a potential issue during the screening, they will refer your child to a developmental pediatrician, child neurologist, or child psychologist or psychiatrist to undergo a comprehensive evaluation and diagnosis.
Common symptoms of ASD include:
- Difficulty communicating and reading social cues
- Restricted interest in others and social situations
- Repetitive or ritualistic behaviors
- Delayed speech and language skills, such as not responding to their own name
- Refusal to acknowledge or point at moving objects (at 14 months)
- No interest in playing pretend (at 18 months)
- Repeating words and phrases
- Avoiding eye contact
- Compulsive physical behaviors like rocking back and forth or hand waving
- Hyperactivity
- Impulsivity
- Difficulty paying attention
- Irritability, prone to aggression or tantrums
- Tendencies to self-injury or self-harm
- Abnormal eating or sleeping patterns
To receive a diagnosis, several of these symptoms must initially present during your child’s early development, not be the result of another condition, and be serious enough to significantly impair their social or academic life.
The earlier a child is diagnosed with ASD, the better. Parents can begin working with health professionals, caregivers, teachers, and other adults who interact with their child to ensure they receive proper accommodations in school and outside the home.
What is ADHD?
Previously known as ADD (attention deficit disorder), ADHD (attention deficit/hyperactivity disorder) is an intellectual disorder marked by hyperactive, impulsive, and inattentive behaviors that interfere with the individual’s functioning. Children with ADHD have difficulty staying organized and regulating their thoughts, emotions, and behaviors.
The DSM-5 categories ADHD into three presentations: predominantly inattentive, predominantly hyperactive-impulsive, and combined presentations. Depending on their presentation, individuals with ADHD primarily display symptoms from one of the below lists (or both, in the case of the combined presentation):
| Inattentive presentation of ADHD | Hyperactive-impulsive presentation of ADHD |
| Difficulty staying focused
Difficulty organizing tasks Difficulty paying attention Avoiding tasks that require sustained focus Difficulty following instructions or finishing tasks Prone to be forgetful or lose things Prone to make careless mistakes or ignore details |
Rash decision-making
Low self-control Interrupts frequently Squirms, taps, or fidgets often Difficulty sitting still Impatient and difficulty waiting their turn Talks excessively Extreme restlessness Difficulty staying quiet when necessary |
ADHD can be diagnosed as young as age 4. Physicians, mental health professionals, and clinical social workers will work with the parent beforehand for a screening interview. Then, they’ll conduct a diagnostic interview with the child to recognize symptoms of the disorder or other comorbid conditions like depression, anxiety, and sleep disorders.Diagnosing children with ADHD Doctors still do not know what causes ADHD. Current research is centered around genetics, premature birth, brain abnormalities, and exposure to alcohol, tobacco, or lead during pregnancy as possible causes. Despite popular misconception, ADHD is not caused by a high-sugar diet or socio-environmental factors.
For a child to be diagnosed with ADHD they must meet the following conditions:
- Display six or more symptoms from either the inattentive or hyperactive-impulsive presentation of ADHD;
- Exhibit these symptoms to a disruptive extent in their lives, for a period of 6 months or more;
- Exhibit several of the symptoms before age 12;
- Exhibit the symptoms in multiple settings (school, home, extracurricular); and
- Not have the symptoms as a result of another mental disorder.
1Significantly different from girls within the same age group (p < 0.05).
2Significantly different from all children aged 6–11 (p < 0.05).
3Significantly different from all children aged 12–17 (p < 0.05).
4Significantly different from children of the same sex aged 6–11 (p < 0.05).
5Significantly different from children of the same sex aged 12–17 (p < 0.05).
NOTES: Data are based on household interviews of a sample of the civilian noninstitutionalized U.S. population. ADHD is attention deficit hyperactivity disorder.
SOURCE: CDC/NCHS, National Health Interview Survey, 2011–2013.
Source: CDC
Part of the trouble with diagnosing ADHD is that symptoms can often be confused with “normal” behaviors during early childhood, or masked by sleep deprivation. For example, children who are sleep deprived may become hyperactive; act impulsively and show low self-control; be irritable, moody, or stubborn; or become inattentive or easily distracted and make careless mistakes. However, these are all symptoms of ADHD as well, whether or not the child is sleep deprived.
When a child presents these symptoms without sleep deprivation, along with other ADHD symptoms, such as difficulty organizing tasks, paying attention, or sitting still, it may be time to seek out a professional for a diagnosis.
Common sleep issues with ASD and ADHD
As many as 80 percent of children with ASD have difficulty falling and staying asleep, and up to half of children with ADHD experience sleep issues.
Problematically, many symptoms of ADHD and ASD contribute to, or are exacerbated by, sleep issues common to children with either or both disorders. Fortunately, some of these issues, such as night terrors or bedwetting, go away with childhood, but some issues like insomnia persist into adulthood.
Below is a list of sleep issues frequently experienced by children with ASD or ADHD. The third column notes conditions shared by both.
| ASD | ADHD | Both ASD and ADHD |
| Insomnia (difficulty falling and staying asleep)
Fragmented sleep Early morning waking Difficulty waking up Sleep-disordered breathing and sleep apnea Short overall sleep time Anxiety around bedtime Excessive daytime sleepiness Parasomnias such as sleepwalking or nightmares and/or night terrors Dyssomnias like restless legs syndrome, periodic limb movement disorder, or rhythmic movement disorder Bed-wetting (enuresis) |
Insomnia (difficulty falling and staying asleep)
Fragmented sleep Difficulty waking up Sleep-disordered breathing and sleep apnea Anxiety around bedtime Excessive daytime sleepiness Parasomnias such as sleepwalking or nightmares and/or night terrors Dyssomnias like restless legs syndrome, periodic limb movement disorder, or rhythmic movement disorder Delayed sleep-phase disorder |
Insomnia (difficulty falling and staying asleep)
Fragmented sleep Difficulty waking up Sleep-disordered breathing and sleep apnea Anxiety around bedtime Excessive daytime sleepiness Parasomnias such as sleepwalking or nightmares and/or night terrors Dyssomnias like restless legs syndrome, periodic limb movement disorder, or rhythmic movement disorder |
Below we will review each of these sleep problems and how they affect children with ASD or ADHD.
Insomnia
Children with ASD are 2 to 3 times likelier to have insomnia than their peers, and children with ADHD are twice as likely. The percentage of children with ADHD who have trouble falling asleep (sleep-onset insomnia) is 15 percent; that number rises to 50 percent during their teenage years. Children with ADHD have difficulty calming down their thoughts and relaxing enough to fall asleep, so it can take them as long as an hour to finally fall asleep. Children with autism may develop resistance around bedtime, making it tough for them to similarly settle down and fall asleep.
Fragmented sleep
Once they fall asleep, both children with ASD and/or ADHD experience restless sleep (sleep-maintenance insomnia) and wake during the night, perhaps due to a co-morbid sleep issue we’ll describe below. Children with ADHD in particular toss and turn often during the night. Children with ASD are also highly sensitive to sensory stimuli, so they’re prone to wake up from even light noise or movement during the night.
Early morning waking
Waking up early is a problem for children with ASD due to their high sensitivity. Light from the sun or noises from outside and within the house wake them earlier than others sharing the home. Such restless sleep prevents them from getting an adequate amount of REM sleep, causing them to spend more in light sleep which in turn is easier to wake from.
Difficulty waking up
Because their sleep is less restful, and they fall asleep later than their peers, both children with ADHD and ASD have a tough time waking up in the morning. They’re less well rested overall, and experience daytime sleepiness as a result. One study found 45 percent of children with ASD had difficulty waking in the morning.
Sleep-disordered breathing and sleep apnea
Sleep-disordered breathing describes abnormal breathing during sleep, including snoring and obstructive sleep apnea (OSA). With OSA, an individual’s airways become blocked during sleep, causing them to stop breathing, so their brain wakes them up to get them breathing again. However brief these apneic episodes, they result in fitful sleep. Sleep apnea affects 3 percent of the general population, 25 percent of autistic children, and nearly a third of individuals with ADHD. Obesity is also highly correlated with sleep apnea, and occurs twice as often in children with ADHD.
Short overall sleep time
Autistic children get roughly 30 minutes less of sleep per night than their peers. Quality sleep helps the brain form memories, consolidate learnings from the day, and regulate a host of other bodily functions. When an individual is sleep deprived, they have difficulty managing their emotions and focusing during the day. These effects of sleep deprivation can compound the developmental delay many children with autism already deal with.
Anxiety around bedtime
Many children are afraid of the dark, but children with ADHD and ASD have more bedtime anxiety than their peers. Children with ADHD have challenges quieting the anxious thoughts racing in their minds before bed, whether from homework, stresses of the day, or anxiety and depression (common co-morbid conditions of ADHD). Autistic children have trouble reading social cues, so when bedtime comes, it can feel like a shock to them even though other individuals in the house have been clearly preparing for bed. This sudden change can be distressing to them. Autistic children also resist sleeping alone more intensely than their typically developing peers. On top of all of this, sleep deprivation caused by their other sleep problems can make children with ADHD or ASD more irritable and prone to throw tantrums before bedtime.
Excessive daytime sleepiness
Because they experience less restful sleep, and less sleep overall, children with ADHD and ASD are often drowsy during the day. This interferes with their ability to focus in school and regulate their emotions, further hampering their ability to form successful social relationships, especially in the case of autistic children.
Parasomnias such as sleepwalking or nightmares and/or night terrors
Both children with ADHD and ASD experience a higher rate of parasomnias, including sleepwalking and nightmares or night terrors. Up to 50 percent of autistic children experience one of these. Fortunately, the vast majority of these parasomnias go away before age 10 or earlier. However, in the case of autistic children, being unable to communicate their fear can heighten their anxiety and complicate their parents understanding what needs to get treated.
Dyssomnias like restless legs syndrome, periodic limb movement disorder, or rhythmic movement disorder
The dyssomnias affecting children with ASD or ADHD make it challenging to fall and stay asleep. Restless legs syndrome (RLS) causes an uncomfortable tingling or numbing sensation in the lower limbs when the person is lying down, accompanied by an irresistible urge to move them to get relief. RLS affects up to 10 percent of the general population, but an alarmingly high rate of 50 percent of individuals with ADHD. Periodic limb movement disorder is a similar disorder when the individual’s limbs twitch strongly enough during sleep to wake them up. Rhythmic movement disorder is more common among autistic children, but goes away by age 5. With this dyssomnia, the person rhythmically rocks their body or head for short episodes (15 minutes or less) while they’re falling asleep.
Delayed sleep-phase disorder
Individuals with ADHD are more prone to have delayed sleep-phase disorder. Children with this disorder have an asynchronous circadian clock and sleep-wake patterns, which cause them to get tired and wake up later than others. This contributes to their anxiety around bedtime because they’re not tired, as well as their sleepiness during the day, because they wake up earlier than they would naturally.
Bed-wetting (enuresis)
Bed-wetting is more common among autistic children, especially those with Asperger syndrome. Bedwetting episodes can wake them during the night and worsen bedtime anxiety, for fear it will happen again.
What causes sleep problems in children with ASD and/or ADHD?
While researchers still do not know what causes ASD or ADHD-sleep related issues in children, they have narrowed it down to a few likely culprits: medication side effects, comorbid health conditions, and genetic abnormalities that disrupt the circadian clock.
Medication side effects
While the CDC strongly recommends behavioral therapy first, many children still end up using medication to treat symptoms of ASD or ADHD. Many ADHD medications are stimulants and known for causing insomnia or disturbed sleep. Children with ADHD or ASD may take SSRIs to treat comorbid depression and anxiety, which are also linked to disturbed sleep and may cause hyperactivity before bed. Drowsiness is another common side effect of ADHD medications and antipsychotics prescribed to children with ASD.
Co-morbid health conditions
Children with ADHD and ASD are more likely to have mental health disorders like depression and anxiety, which independently contribute to insomnia and restlessness before bed. Certain health problems are also correlated with ASD or ADHD, such as epilepsy and acid reflux in the case of ASD. These interfere with sleep, and the side effects of their medications may impact it as well.
Genetic abnormalities
Children with ASD exhibit inverse melatonin production, a hormone critical to regulating sleep. Their levels peak in the morning instead of at night like other people, which impacts their sleep-wake cycle.
Helping children with ADHD and ASD sleep better
While children with ADHD and ASD suffer from more sleep issues than their peers, the good news is that there is a variety of behavioral therapies, sleep products, and medications to help alleviate these issues.
Implementing just a few of these may greatly improve your child’s sleep, which will in turn have a vastly positive effect on their day-to-day life. A 2006 study reviewed that autistic children who slept better had fewer behavioral issues in school and improved social interactions. A 2010 study of Japanese children found similar improvements for children with ADHD, who napped less during the day and experienced lower rates of problematic behaviors.
Behavioral treatments
The first step to helping your child fall asleep is establishing a bedtime routine. The key to a successful bedtime routine is consistency.
Every night, in the 30 to 60 minutes before bedtime, follow the same activities in the same, calm order: taking a bath, brushing their teeth, and reading a bedtime story, for example. Children may find a reward system encouraging, but avoid upsetting them when they fail by reminding them they can always try again tomorrow to be successful. Autistic children may benefit from visual cues such as pictures that accompany steps of the routine.
Children should also learn to fall asleep on their own, so gradually coach them by spending a few days sleeping in their bed, then next to their bed, then in a chair, until you finally move out of their bedroom completely.
Next, practice good sleep hygiene. This includes avoiding stimulating activities in the hours before bedtime, and making the bedroom a calm, relaxing environment conducive to sleep. Help teenagers organize their homework and other commitments so they don’t go to bed stressed out. Set the bedroom thermostat to a cool mid-60 degrees Fahrenheit. Make sure your child’s pajamas and bedding are soft to touch and don’t have any itchy tags, especially if your child is autistic and highly sensitive.
Remove electronics from the bedroom. The American Academy of Pediatrics revealed the presence of a TV or a computer can negatively affect an autistic child’s sleep, compared to peers with ADHD or typical development (TD).

Consider adjusting your child’s exercise and diet. Exercise should be completed hours before bedtime. Avoid snacks that might upset their stomach in the early evening, especially if you have an autistic child with acid reflux. Instead, provide bedtime snacks using foods known to facilitate sleep through a high tryptophan or natural melatonin content. These include nuts, dairy, cherries, bananas, and beans. Avoid caffeine, stimulants, and junk foods high in sugar.
If the above don’t provide adequate relief for your child’s sleep issues, you can try various sleep therapy programs, including:
- Cognitive behavioral therapy has proven very effective for children with insomnia. Psychotherapists explain the importance of sleep and help children recognize and learn to regulate their thought patterns so they can calm their thoughts and anxious feelings around bedtime.
- Relaxation exercises may be included in CBT or practiced separately. Meditation and deep breathing exercises help calm children, such as lightly rubbing their back in a consistent rhythm as they breathe deeply.
- Light therapy helps individuals with out-of-synch circadian clocks adjust to a typical sleep-wake cycle. This is helpful for autistic children as well as children with ADHD and delayed sleep phase syndrome. Children sit in front of a bright artificial light box for a set amount of time in the morning or at night, depending on whether they need help waking up or staying awake.
Sleep products
- Both children with ADHD and ASD can be easily distracted while falling asleep, from racing thoughts or anxiety in the case of ADHD, or from being highly sensitive to environmental stimuli in the case of ASD. White noise machines release a static sound that can lull your child to sleep and block out other noises.
- Earplugs, eye masks, and blackout curtains can help autistic children further block out external stimuli like noise from a creaking door hinge or light from the sun in the morning.
- Anti-snoring mouthpieces, chinstraps, pillows, and nasal plugs can alleviate snoring and sleep-disordered breathing. Children with severe sleep apnea can get fitted for a continuous positive air pressure (CPAP) machine.
- Weighted blankets can soothe symptoms of RLS, as can iron supplements if the RLS is caused by an iron deficiency. Weighted blankets should weigh 10 percent of your child’s body weight plus 1 pound.
- Waterproof mattresses and bedding can make cleanup easier for parents of autistic children prone to bedwetting. They’re made from easily cleanable materials that don’t develop stains or an odor, even with repeated incontinence.
- Padded bed rails and/or floor pads can keep children with night terrors, rhythmic movement disorder, or autism-related epilepsy from hurting themselves during sleep. A padded bed rail keeps them in the bed without hitting something too hard, and a floor pad offers additional protection if the rails give the child anxiety.
Medication
22 percent of children with ADHD take sleep medication to help them fall asleep, but scientists are still researching the long-term benefits of safety of it. Children with ADHD or ASD may already be on medications to manage their symptoms, so parents should check with their doctor first before taking additional medication to manage their sleep issues. Otherwise, the side effects can interfere with each other and be dangerous.
One such supplement children may take is melatonin. Taking melatonin before bed can help kickstart melatonin production and induce sleep, but parents should discuss recommended dosage amounts with their doctor, as high dosage amounts have been linked with seizure for children with ADHD or ASD. Typical dosage amounts range from 0.5 to 5mg for children, depending on the severity of their symptoms.
Clonidine and Mirtazapine are two other medications prescribed to children with ASD who suffer from insomnia.
Additional Resources
- If you’re not sure whether your child has ADHD, consult the CDC’s checklist of common warning signs.
- Similarly, the National Autism Association’s First Signs, Next Steps Toolkit helps parents recognize early signs of autism and understand what’s involved in diagnosis, how to get treatment, and find local support groups.
- Autism Speaks is an advocacy organization that funds research and connects families and caregivers with local resources and events. Their Quick Tips guide to improving sleep in autistic children offers detailed instructions and printable visual aids to help children recognize different steps of the bedtime routine.
- The National Resource on ADHD keeps an up-to-date list on the most commonly prescribed medication for ADHD and side effects.
- ADDitude Magazine has over 600 articles on sleep and how it affects ADHD. The magazine is available online and in print and includes an online forum.
- AutisMag is the leading magazine for autism. Their article on sleep problems in children with autism or ADHD provides additional advice for helping your child fall asleep, based on the types of sensory stimuli they respond best to (e.g. tactile or visual).
- The Attention Deficit Disorder Association offers “Sleep Strategies for College Students with ADHD” and related articles, which can be helpful for parents whose children are leaving home for the first time.
- Amazon has Best Sellers sections devoted to books on Attention Deficit & Attention Deficit Hyperactivity Disorder and Autism & Asperger’s Syndrome.
- The UK-based National Autistic Society provides relaxation techniques to help an autistic child sleep better, as well as advice on coaching your child to sleep without you in the room and self-soothe themselves back to sleep if they wake during the night.
- Parents can connect with other caregivers and share their experience on various online forums, including the ADHD subreddit, ADDConnect, ADDForums, Autism subreddit, ASPIESCentral, WrongPlanet, and AutismWeb.
The original publication of this article can be found at – https://www.mattressreviews.net/helping-children-with-adhd-and-asd-sleep/
Editor’s note
Readers might also be interested in reading the guide below on improving quality sleep



